Wellington Eye Centre’s Ophthalmologist
Eduard Zirm completed the first successful corneal graft, also known as a corneal transplant, in 1905. Since then innumerable ophthalmologists have refined and developed the procedure to become the most common and successful form of human transplantation.
This article will discuss some of the reasons people may need a corneal graft, what types of corneal transplants are now possible and what researchers are working on for the future.
What does the cornea do?
First you need to understand the role your cornea has in your vision. It is the front surface of the eye and is responsible for 60% of the focusing power for the eye. The lens provides the other 40% of the focusing power, which lies behind the iris. The cornea has a fixed focusing power, while the lens is able to change its focusing power by changing shape. This allows the eye to focus at different distances.
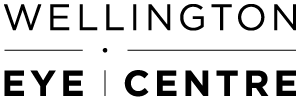
The cornea is normally about 550 microns (0.55mm) thick and consists of 5 layers. Here are the different layers going from the front to the back of the cornea:
- Epithelium or “skin”. This a layer of cells, 5 cells thick on the front of the eye.
- Bowman’s layer. This is a cell-free membrane about 20 microns thick.
- Stroma. This makes up the bulk of the cornea and is about 500 microns (0.5mm) thick. It consists of layers of tough fibres made of a connective tissue called collagen. Special corneal cells called keratocytes are found lying between the layers of collagen fibres.
- Descemet’s membrane. This is a tough, thick membrane made up of collagen.
- Endothelial cells. Lining the inside surface of the cornea and attached to Descemet’s membrane, the layer of endothelial cells is one cell thick. They act as pumps, sucking fluid out of the cornea and preventing it becoming swollen and waterlogged. They are extremely limited in their regeneration.
In order to carry out its normal function the cornea has to be crystal clear and evenly curved in all directions. Anything that affects the normal transparency and curvature of the cornea can interfere with clear vision.
Why would someone need a corneal transplant?
The normal cornea is crystal clear allowing almost perfect transmission of light. Corneal grafts are usually performed because the natural cornea is unable to form a clear image. This can occur due to either a loss of the normal transparency or a change in the shape of the cornea. If glasses or contact lenses cannot restore vision, a corneal graft may replace the distorted or cloudy tissue to improve vision.
What causes loss of transparency?
- Scar formation, following an injury or infection from a virus, fungus, or bacteria. If the scar is peripheral and does not cross the line of sight it may have no effect on vision. However, a central corneal scar, or one that affects the shape of the cornea, is likely to affect vision so that a corneal graft is required.
- Increased water content. To remain crystal clear, the cornea must maintain a low water content. If the water content of the cornea increases sufficiently, it can become swollen and cloudy, a condition known as corneal oedema. Special cells called the endothelial cells which line the back of the cornea maintain the low water content of the cornea. Water continuously enters the cornea from the tear film and these cells act as pumps to suck the water out of the cornea. Injury, surgery inside the eye, ageing and inherited disease may cause or damage or loss of endothelial cells. The cornea can develop oedema if there are insufficient remaining cells to maintain corneal dehydration.
- Blood vessel growth. Normally there are no blood vessels in the cornea. However, they can grow into the cornea following an injury or severe infection. These blood vessels normally have leaky walls and can leak substances such as cholesterol into the corneal tissue causing clouding of the cornea.
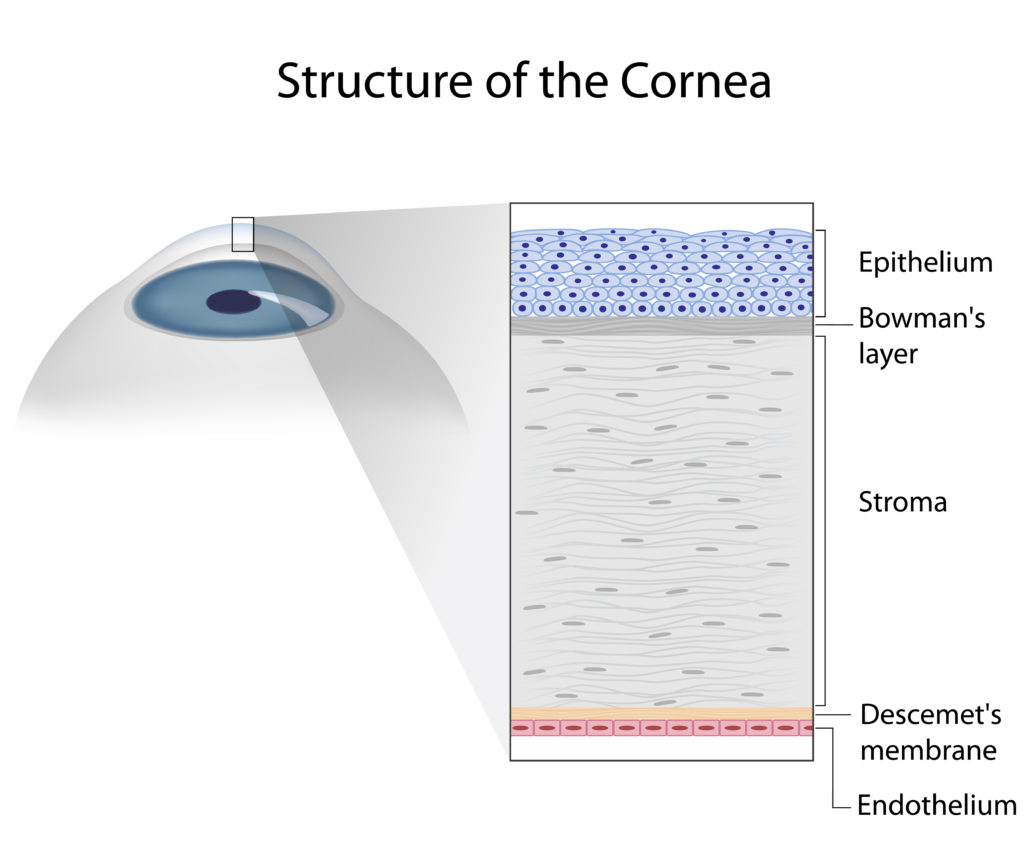
- Changing shape of the cornea. A condition called keratoconus is the most common cause of an abnormally shaped cornea. The cornea develops an area of weakness causing an increasing bulge due to the normal pressure inside the eye. Approximately 2% of the New Zealand population have keratoconus and it is the most common reason for a corneal graft. The cornea may also become distorted due to scarring following an injury or severe infection.
Types of Corneal Grafts
Following almost a century of experiments using animals, mainly rabbits, Eduard Zirm performed the first human corneal transplant in 1905. Initially, all conditions treated with a corneal transplant required a “full thickness” or “penetrating” graft. However, over the last 20 years there have been major advances in how corneal grafts are carried out. Nowadays the type of graft used is dependent on the condition.
Full thickness or penetrating graft
If the lower layers or all the layers of the cornea are damaged, the eye will require a full-thickness graft. A full-thickness graft replaces all layers of the cornea, including the endothelium. This usually requires an operating theatre and general anaesthetic. The need for a full-thickness graft might arise from a severe injury or infection, or if the cornea has become very thin due to advanced keratoconus.
Full thickness grafts can work very well but they have several disadvantages. Replacing all the cornea requires a lot more healing to occur, and it can take over a year before stitches can be removed and vision stabilizes. When stitching the graft tissue it can be difficult to avoid distorting it. The new cornea can then have significant amounts of astigmatism. This then requires the wearing of glasses or contact lenses to obtain useful vision.
Replacing the whole cornea is significant because it means removing the recipients’ own endothelial cells. These endothelial cells will not grow back, they are instead replaced by the endothelial cells already on the graft. The removal of the patients own endothelial cell layer increases the risk for graft rejection, and a full thickness corneal graft carries a lifetime risk of graft rejection. Finally, the healed interface between the graft and patient’s natural cornea never reaches the same strength as a normal cornea. If the eye suffers trauma, even that which would not normally cause a severe injury, the graft can be lost.
Lamellar grafting
Because of the disadvantages of full thickness grafts, new techniques have been developed over the last 30 years. A lamellar graft, means only a layer or lamella of cornea is replaced. Leaving as much as possible of the recipient’s normal corneal tissue in place. This can result in less risk of graft rejection, faster visual recovery, better unaided vision, and a stronger eye that is less vulnerable to injury.
Anterior Lamellar Keratoplasty (ALK)
ALK is usually used to treat corneal scars or opacities affecting only the front of the cornea. The size and thickness of the corneal opacity determines the amount of tissue replaced. The surgeon will attempt to leave as much of the patient’s normal corneal tissue behind to maximise the strength of the cornea after the surgery. By removing only the affected layer of corneal tissue from the patients eye and replacing it with donor corneal tissue.
Previously, the corneal tissue was cut manually or using a mechanical device called a microkeratome. Nowadays, most surgeons who perform ALK will use a femtosecond laser to cut the corneal tissue; the same laser used to perform LASIK and SMILE surgeries. The laser is extremely precise and creates very smooth surfaces in the corneal tissue. You are able to achieve much better visual outcomes than with a microkeratome or manual procedure. In many ALK cases, no stitches are needed, and visual recovery can be rapid with high quality and stable vision being achieved within a few months.
Because only part of the cornea has been replaced, it is much stronger than is the case following a full thickness corneal graft. I, Dr Andrew Logan, from the Wellington Eye centre was the first eye surgeon in Australasia to carry out ALK surgery using a femtosecond laser. ALK procedures generally do not require hospital admission and can be carried out in our laser theatre. The procedure is done using anaesthetic eye drops, a general anaesthetic is not required. If no stitches are needed the procedure takes less than 20 minutes.

Deep Anterior Lamellar Keratoplasty (DALK)
The surgeon removes the front 3 layers of the cornea from the patient, which leaves behind the Descemet’s membrane and the endothelial cells. Graft tissue replaces this section, returning the corneal thickness and structure to normal. A DALK is usually done if the corneal stroma is abnormal but the endothelial cells are normal. Such as occurs in advanced keratoconus. As the graft recipient keeps their own endothelial cells, there is a much lower risk of graft rejection compared to a full-thickness graft.
Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) & Descemet’s Membrane Endothelial Keratoplasty (DMEK)
DSAEK and DMEK are similar procedures which replace damaged endothelial pump cells. The epithelial cells, Bowman’s membrane and stroma of the graft recipient are left untouched. It’s a very thin graft, 100 microns thick or less and about 8mm in diameter; this consists of endothelial cells, Descemet’s membrane and a thin layer of stroma. The graft is inserted inside the eye where it is floated against the back of the cornea. The graft then sticks in place on the back of the cornea, and takes over the pump function of the patient’s abnormal or damaged endothelial cells. DSAEK and DMEK are quite quick operations to carry out, and have a lower risk of graft rejection and faster visual recovery compared to full thickness corneal grafts.
Where does corneal graft tissue come from?
Organ donors. Corneal graft tissue collection is from those who have given consent, prior to death. In most developed countries, Eye Banks carry out donor cornea collection, testing and distribution. They have the necessary skills and equipment to do this.
The New Zealand National Eye Bank in Auckland collects all corneal donor tissue in New Zealand. People who have died from systemic infections or who have had a neurological condition which could be Creutzfeldt-Jakob Disease (CJD) or variant CJD (“mad cow” disease) cannot donate. This is to prevent disease transmission to the graft recipient. Donors are also tested for the presence of HIV and Hepatitis A, B and C, for the same reason.
Despite these advances, corneal graft surgery still requires the use of human donor corneas. Please consider agreeing to be an organ donor on your driver’s license. If you have a family bereavement, offering your loved one’s corneas for donation can give someone the gift of restored sight and a new life.
The future of corneal grafting
In most countries, including New Zealand, there is a chronic shortage of corneal graft donor tissue. Significant research is being carried out in many countries, including New Zealand, to find ways to bypass the shortage of donor corneal tissue.

Use of animal corneal tissue (xenograft)
Animal tissue has been used in human surgery for many years, in particular using heart valves from pigs to replace damaged human heart valves. A lot of laboratory investigation has been carried out investigating the potential use of pig corneas as a substitute for human corneas in corneal grafting. However, there are significant ethical issues and concerns about possible disease transmission from animals to humans, and no procedures of this type have been carried out. New research and developing techniques make it very unlikely that animal tissue will ever be used in corneal grafting.
Tissue engineered corneas and 3d printed corneas
Huge advances in the last few years using 3D printing and tissue engineering means rocket engines to working mouse hearts can now be produced by 3D printing. Scientists have even made artificial corneas which are able replicate the size, shape, structure and function of normal human corneas and are probably only a few years away from becoming available for human use. They will revolutionise corneal transplant surgery by providing cheap, safe, and disease-free artificial corneas in unlimited quantities.
Stem cells
Research into developing the use of stem cells to replace cellular components of the cornea, particularly the endothelial cells is happening worldwide. We are now at the stage where stem cells taken from a patient can be reliably transformed into corneal endothelial cells. These can then replace abnormal endothelial cells instead of having a DSAEK or DMEK graft. This technology is potentially only a few years away from being used routinely in human surgery.
If you have any other questions feel free to get in touch with the team at Wellington Eye Centre. You can call us on 0800 733 327 or complete the contact form below.

Amblyopia and Laser Eye Surgery

What are the visual requirements to join the Police in NZ?
What Can Go Wrong During Your Laser Eye Surgery?

What are the visual requirements for flying, set by the Civil Aviation Authority?

What happens when your vision after laser vision correction surgery is not what you expected?

Everything You Need To Know About Dry Eye

What to expect during your Laser Suitability Medical Assessment at Wellington Eye Centre

Low-Level Light Therapy for Dry Eyes

Common Medications Used in Laser Eye Surgery