Macular Degeneration affects an estimated 14% of New Zealanders over the age of 50. What is macular degeneration, how do the symptoms present, and what treatments are available?
What is Macular Degeneration?
Macular Degeneration is a condition in which the macular tissue of the eye starts to deteriorate or degenerate, causing progressive loss of central vision.
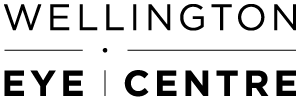
In understanding this condition, it is helpful to know a bit more about the anatomy of the eye, read on.
What is the Macula?
It can sometimes help to compare the eye anatomy to the parts of a digital camera.
The eye’s equivalent to the camera’s sensor is a tissue called the retina. With a camera, the image or light passes through the lens, and is focused on the camera’s sensor. With the eye, the image and light also pass through a lens, to be focused on the retina.
The retina is a thin membrane, it lines the inside of the back of the eye. The retina is connected to the visual cortex in the brain via the optic nerve. (see the diagram above).
The eye has cells called photoreceptors, which are light detecting cells. They act like pixels in a digital camera. There are different types of photoreceptors in different areas of the retina.
The photoreceptors in the outer parts of the retina have poor colour perception and relatively low resolution. This is why our peripheral vision is not as clear as our central vision. Our peripheral vision is more attuned to detecting movement, rather than detail.
The centre of the retina, is called the macula. The macula lines up with the centre of the pupil. The photoreceptors in the macula are densely packed and can detect colour and provide high quality vision. The macula is only about 2 millimetres in diameter but is responsible for all of our detailed and colour vision.
When you look straight at an object such as a page of print, the image of that print falls directly onto the macula. This is why a healthy macula is so important for good vision. Macular degeneration occurs when the tissues (including the photoreceptors) of the macula are damaged.
Types of Macular Degeneration?
The most common form of macular degeneration is called Age-Related Macular Degeneration (ARMD or AMD), although a similar condition can occur in younger people as well.
ARMD is one of the most common causes of vision loss in older people. About 14% of people over the age of 50 will have signs of early macular degeneration, but only a few of those people will have their vision severely affected. Over the age of 75, about 30% of people have signs of early macular degeneration and 2% to 3% of people will be severely affected.
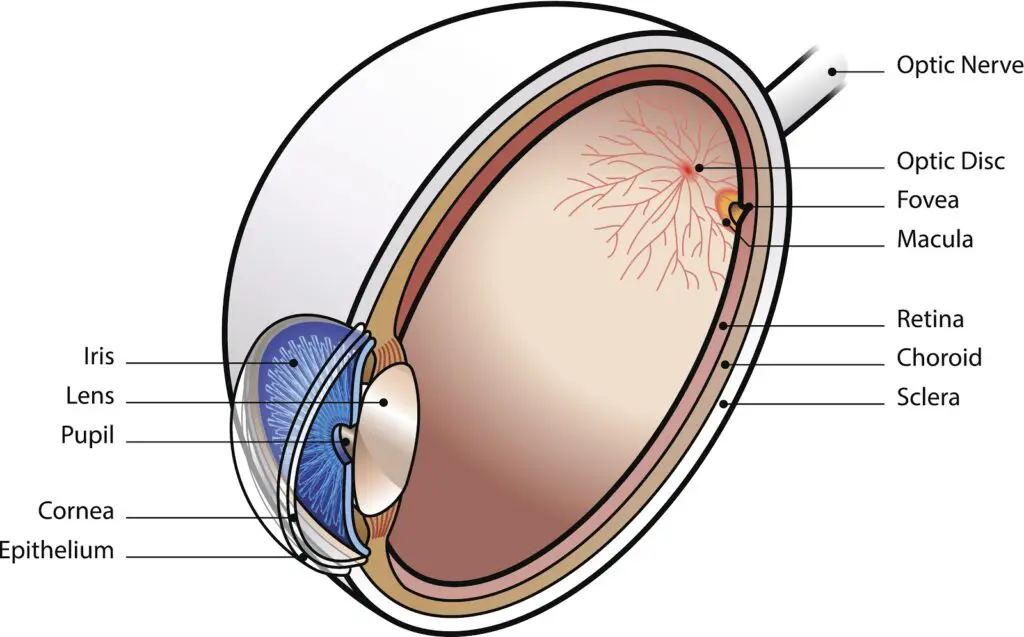
There are two types of Age-Related Macular Degeneration – wet and dry.
Dry Age-Related Macular Degeneration
Dry macular degeneration is the most common type of macular degeneration. It develops slowly over many years. The degeneration is caused by damage and loss of cells underlying the retina. As the cells in and under the retina slowly die, vision becomes progressively poorer.
Wet Age-Related Macular Degeneration
Wet ARMD occurs when abnormal blood vessels grow under and in the retina, in the area of the macula. These blood vessels leak fluid and blood under the retina, causing damage to the central vision.
Unlike Dry ARMD, which develops slowly, Wet ARMD can progress rapidly to the point where vision is severely affected.
What causes Age-Related Macular Degeneration?
The causes of ARMD are not fully understood, but multiple factors can contribute to the development of macular degeneration. ARMD is the subject of a lot of laboratory and clinical research.
Several genetic mutations have been identified as risk factors for the development of ARMD, however at present, there are no gene therapies available for treating ARMD.
Increased age and a family history of ARMD had been identified as significant risk factors for developing ARMD, but unfortunately, neither age, family history nor genetics can be modified.
The single most important modifiable risk factor for ARMD is smoking, and this is yet another reason to quit if you smoke.
What are the symptoms of Macular Degeneration?
ARMD can affect vision in several ways, and some of these symptoms will vary depending on whether it’s Dry or Wet ARMD.
Dry ARMD may cause blurred, fuzzy vision or blind spots in the central vision. If both eyes are affected to a different degree by the ARMD, the visual deterioration may not be picked up. If vision is still good in one eye, then this may compensate for deteriorating vision in the other eye, making it harder to notice.
Wet ARMD can also cause blurred or fuzzy central vision, but because the leaky blood vessels underneath the retina cause distortion of the retina, it can also cause bending and distortion of straight lines.
So in summary, look out for the following symptoms:
- blurred or fuzzy central vision
- dark or blank spots in your central vision
- distorted lines, which are expected to be straight
- loss of fine vision
- decrease in the intensity of colours
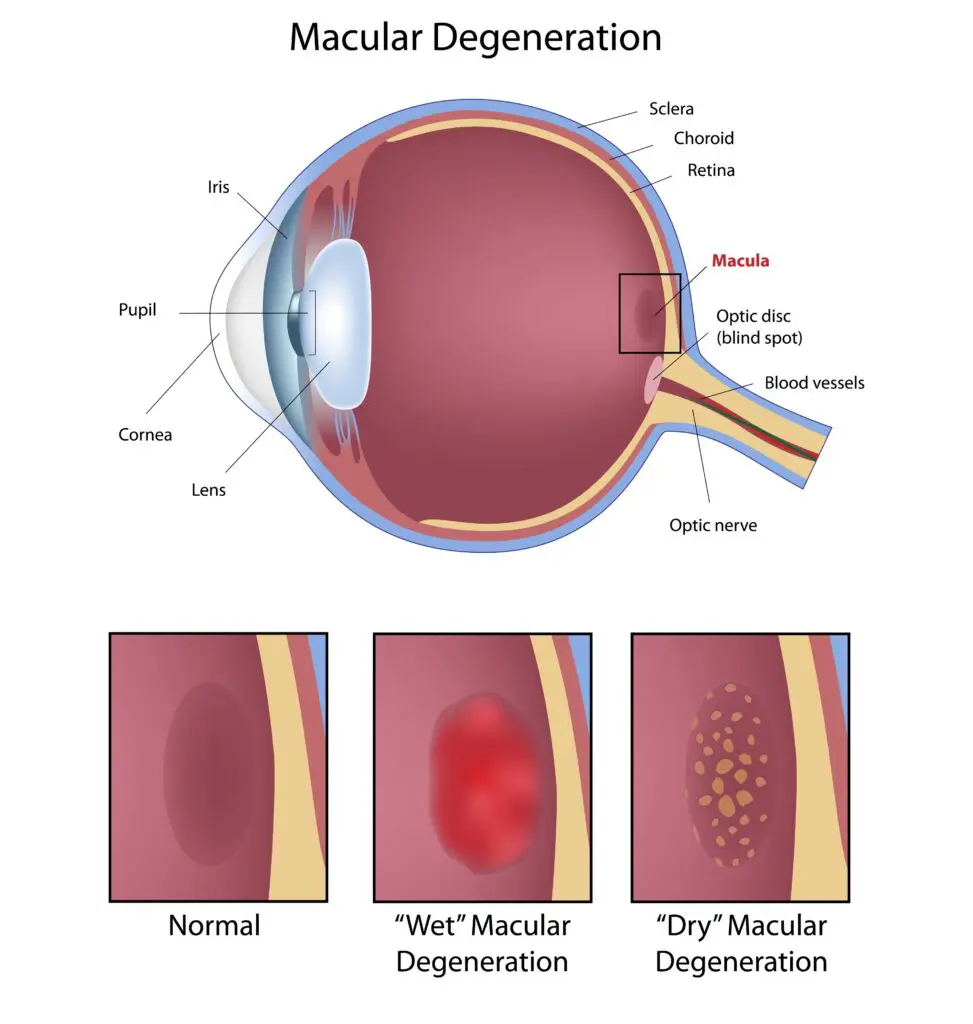
This is what blurred or fuzzy central vision could look like:

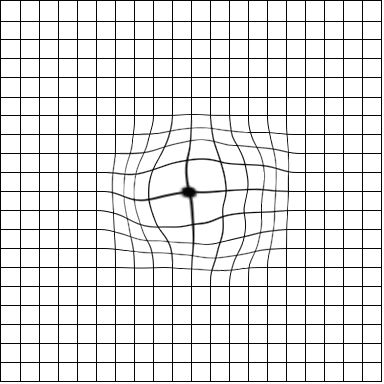
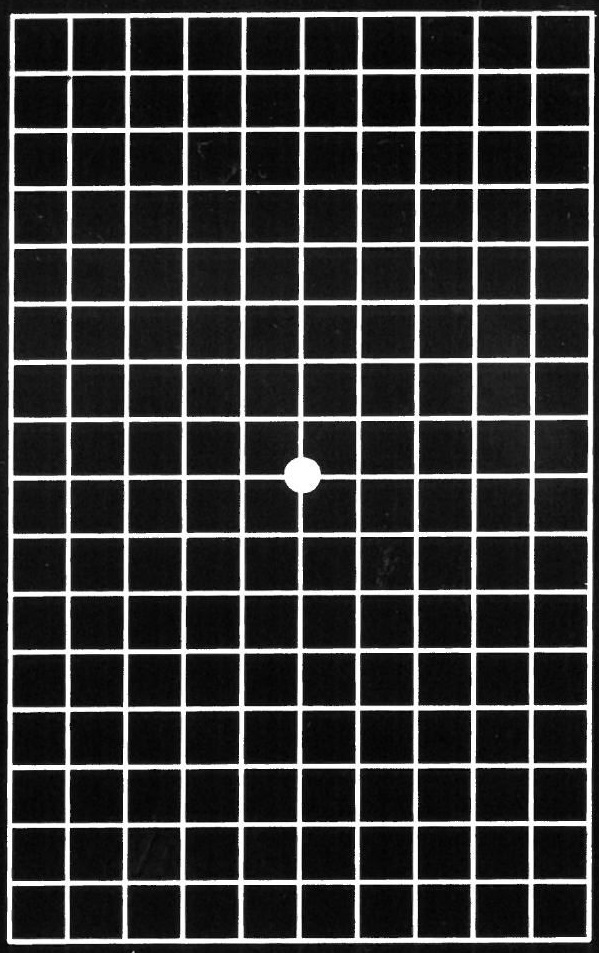
Straight vertical or horizontal lines may appear distorted, like the image below:
Similar symptoms may be experienced by people who don’t have macular degeneration but may have a macular hole. A macular hole usually develops over time and is caused by the vitreous pulling on the retina. They can be surgically treated with a procedure called vitrectomy. The sooner macular holes are treated, the more effective the treatment and visual outcomes.
How is Age-Related Macular Degeneration diagnosed?
Our ability to diagnose ARMD has improved dramatically in recent years. This is because the technology for imaging the layers of the retina has improved. However, older and simpler methods of diagnosing ARMD are still very useful.
In somebody over the age of 60, deteriorating vision may be an early sign of developing ARMD. It’s important to have regular eye checks with an ophthalmologist or optometrist to see if ARMD is developing.
The eye care provider will usually examine the retina using a microscope and special lenses. If they detect any signs of ARMD, they may need to carry out further tests. The most common diagnostic test carried out for detecting ARMD is called an OCT, which stands for Ocular Coherence Tomography. An OCT machine uses infrared light to image layers of the retina. It can easily detect the signs of Dry and Wet Macular Degeneration, and can also be used to assess if the ARMD is getting worse, or to monitor the effect of any treatment.
People who have ARMD present, even mild cases that don’t have any significant vision issues, still require regular follow-ups. This will involve checking your vision and examining the retina with a microscope or using an OCT scan. It’s important to continue getting these check-ups in case the ARMD progresses, even subtle changes might be a sign that a new treatment or intervention is required, so don’t ignore any symptoms, get your eyes checked regularly!
Tips for managing ARMD yourself at home
There are several things you can do to monitor your vision if you’ve been told you have ARMD. You should check the vision in each of your eyes separately a couple of times a week. Testing both eyes together can mask a significant loss of vision in one eye. You can do this while reading a newspaper or a book with normal-sized print. Cover one eye at a time and observe what your vision is like. If you notice a blind spot, distortion, or bending of straight lines, and this has not been present previously, it could be due to a recent or rapid development of Wet ARMD. You should see your ophthalmologist as soon as possible.
Your eye care provider may also give you something called an Amsler Grid. This is usually a sheet of A5 white paper with a grid of straight black lines and a dot in the middle (like the earlier image). By looking at the dot in the centre of the grid with one eye open and the other closed, any distortion or blind spots can be easily detected. This method can be used to help monitor your vision and potential changes relating to ARMD.
It’s particularly important to monitor your vision if you have been told that you have, or are at risk of developing Wet ARMD. There are now several treatments available which can effectively reduce the severity and stop the progression of Wet ARMD. However, these treatments are much less effective if treatment is delayed.
How to use the Amsler Grid to check your vision
- While wearing your usual glasses, place the Amsler Grid at reading distance (about 35 – 40 centimetres from your face).
- Make sure there is good light while you do this.
- Cover one eye
- Look at the centre dot
- Note irregularities (wavy, size, grey, fuzzy)
- Can you see the four outer corners of the grid.
- Test the other eye
- If you notice any irregularities contact your ophthalmologist or optometrist
Treatment of Age-Related Macular Degeneration
Treatment of ARMD starts with the prevention or reduction of risk. Smoking is an important modifiable risk factor for developing ARMD, and this is a good reason never to start smoking or to stop smoking if you already do so. If you have been told that you have early ARMD, it is a good idea to take a multivitamin based on the findings in the AREDS study. Your ophthalmologist will tell you which one to use.
Treatment of Dry ARMD
Most websites will say there isn’t currently any treatment available to stop or reverse the progression of Dry ARMD. Only treatments to slow the progression of the condition.
A large study in the United States (known as the AREDS study – Age-Related Eye Disease Studies), involved giving a specific multivitamin preparation to people with ARMD. The study suggested that these multivitamins could slow the progression of Dry ARMD. Dry ARMD can sometimes progress to Wet ARMD, and the study suggested that the multivitamin may reduce the chance of this progression.
Photobiomodulation Therapy
A new treatment, recently introduced to New Zealand, has also shown promise in slowing the progression of Dry ARMD. Some trials have shown that study participants had a small improvement in vision after the treatment. This treatment is called Photobiomodulation (PBM) therapy, which uses low-level light to penetrate the eye to reach the cells and tissue in the macula. Once it reaches these cells, it targets mitochondria cells, encouraging cell function, reducing inflammation and decreasing oxidative stress, all of which are elements in the progression of the condition. PBM therapy is non-invasive and has minimal negative side effects. The Wellington Eye Centre already offers Low-Level Light Therapy for dry eye treatment and plans to introduce PBM Low-Level Light Therapy for Dry AMD later in 2026.
Treatment of Wet ARMD
When it comes to Wet ARMD, there are several well-established treatments available. Laser treatment has been used for many years to dry up the blood vessels growing under the retina; which cause retinal damage and Wet ARMD. This laser treatment is not to be confused with refractive laser eye surgery, it is a very different procedure. There are also several medications, called monoclonal antibodies or biologic agents have been developed to treat the blood vessels. These medications are now the go-to treatment for wet ARMD. These medications appear to be more effective and result in potentially better vision than laser treatment. Both these treatments are available in public hospitals and private clinics. Your eye care provider can refer you for treatment accordingly.
All of the treatments used for Wet ARMD are more effective if they are performed before the condition becomes too advanced. In situations where treatment is delayed, they may not offer any benefit at all. For this reason, if you have been told that you have any signs of Dry ARMD or Wet ARMD, it is very important that you monitor your vision regularly. Contact your ophthalmologist immediately if you notice a change or deterioration in your vision. Use the Amsler grid to check your vision two-three times a week or as often as your eye specialist has asked you to.
More Information
You can also find more information on the Macular Degeneration New Zealand website, including a list of optometrists and ophthalmologists in your area, who specialise in macular degeneration. Blind Low Vision NZ also provides information and support for partially sighted people, including help with practical daily life issues and counselling support.
Feel free to get in touch with the team at Wellington Eye Centre if you have any other questions or wish to book a consultation with Dr Logan. You can call us on 0800 733 327 or complete the contact form below.

Everything You Need To Know About Dry Eye

Low-Level Light Therapy for Dry Eyes

Amblyopia and Laser Eye Surgery

Marijuana’s effect on the eyes

Festive Season and Your Eyes

Age Related Macular Degeneration (ARMD)

Wellington Eye Centre Sustainability | How We Reduce Waste & Support the Environment

Everything You Need To Know About Dry Eye

What to expect during your Laser Suitability Medical Assessment at Wellington Eye Centre