Wellington Eye Centre Optometrist
The effect migraines can have on your eyesight is both fascinating and disruptive. But the very first time you experience it, it can also be very distressing. In this blog, we explore the connection between the brain, the eyes and what we see.
What is a migraine?
A migraine is a recurrent and severe headache which a whopping one in ten New Zealanders suffer from. There are a few different types of migraines which people usually experience:
- A classic migraine occurs in about 40% of migraine sufferers and has an aura (visual, auditory, olfactory or tactile).
- A common migraine occurs in about 60% of migraine sufferers and has no aura.
- A silent migraine is when a person experiences the aura, but no headache or pain afterwards.
- A visual migraine is a silent migraine when the aura is visual.
- A retinal migraine is very rare and its visual symptoms are the partial or total loss of vision, temporarily in one eye. In recurrent cases, it is most likely to affect the same eye each time. The vision fades out over five minutes, and can be described as a dimming of vision, flashes of light or patches of blank spots (scotomas) that enlarge to block out all sight in that eye. The vision returns to normal within an hour. This loss of vision is caused by reduced blood flow or spasms of the blood vessels in the retina or behind the eye, not in the brain.
Migraines might occur rarely, once or twice a year, or they could strike several times a month. The frequency differs drastically between sufferers and is often associated with an underlying cause. Migraines usually run in families as they have a genetic component. People with two parents who suffer from migraines have a 75% chance of having migraines themselves. Women are also three times more likely than men to get them.
What are the symptoms of a migraine?
Migraines affect people in different ways but the most commonly described symptoms are;
- Throbbing pain or pulsing sensation on one side of the head
- Severe pain typically lasting 4 – 72 hours
- Aura occuring for 10 – 30 minutes, up to one hour before the migraine pain starts
- Extreme sensitivity to light, noise and sometimes to smell and/or touch
- Vomiting and/or nausea
What is an aura?
Aura is a sensation that occurs before the migraine. It can also occur before other brain conditions too, like seizures. In a migraine, the most common auras are visual; flashing lights, zig zag patterns, blurred vision or patches of shimmering light. Often described as psychedelic in appearance. Other auras can be olfactory (the smell of smoke or rotting food), auditory (ringing in the ears) or physical like the feeling of a breeze, numbness, weakness or difficulty speaking.
What causes migraine pain?
Research is still ongoing, but migraines are thought to likely be caused by a phenomenon called cortical spreading depression (CSD). This is a process that happens in the brain, more specifically the cortex, when these brain cells are over stimulated.
This stimulation affects the production of serotonin and other brain chemicals. Serotonin then stimulates the trigeminovascular system. This system controls the brain’s blood vessels, causing them to swell.
Swollen blood vessels do two things:
- Push on neighbouring nerves – causing the sensation of pain.
- Force the blood to travel through much smaller than normal spaces, making the pulsation of the blood more prominent.
With changes like this happening to the vessels inside our heads, it isn’t all that surprising that people often describe the pain as throbbing or as a feeling of pressure inside their head.
What is a migraine trigger?
Most migraine sufferers learn what their triggers are. A trigger is an action or event that tends to lead to the migraine starting. Sometimes a person needs to have a combination of triggers to occur before they get a migraine.
Some common triggers include:
- Lack of or too much sleep
- Skipped meals
- Bright lights, loud noises, or strong odours
- Hormone changes during the menstrual cycle, pregnancy, menopause or puberty
- Stress and anxiety
- Weather changes
- Physical exertion
- Certain foods; such as red wine, chocolate, caffeine or aged cheese
For many sufferers, no trigger can be found.
What is a visual disturbance?
A visual disturbance is how we describe a change to your vision that is not normal. This term is most commonly used when describing the visual symptoms seen with migraines.
What do visual disturbances look like?
- Black spots, threads, wiggly lines that float across your vision. We call these floaters. This visual disturbance can occur with or without flashes of light.
- Patches of shimmering light or flashing lights.
- Psychedelic colours, distorted colours and shapes, or kaleidoscope vision.
- Zig-zag patterns or dark spots in your vision.
These are all associated with visual aura of migraine.
What to do if you have a visual disturbance
If you are suffering from visual disturbances;
- Stop what you are doing. If you are driving, pull over as soon as you can do so safely.
- Stay calm. Most visual disturbances will pass in 10-30 minutes and are not likely to be a medical issue.
- Rest, often a cool dark room is most comforting.
- Take paracetamol, ibuprofen, diclofenac or naproxen – whichever painkiller you have previously used comfortably and safely.
- Record, write down what you feel and see. Take special note of whether or not the disturbance is affecting one or both eyes.
Then, when you get a chance, contact your Optometrist or GP to discuss how soon you should be checked. In most cases these symptoms are not urgent.
But if you have sudden loss of sight in one or both eyes, or in a section of your vision, seek medical advice immediately.
Why does a migraine affect vision?
While the exact causes of migraine and aura are not fully understood, we are aware of what happens to the brain after a migraine is triggered. The “cortical spreading depression” or over-stimulation of the brain has a flow on effect.
This sudden intense activity in the brain cells is like if all the lights in a city were turned on at once. Then it is followed by a drop-off of activity in that area of the brain. Like a power cut, a blackout in one suburb of the city. The decrease in activity spreads across the top layer of the brain (the cortex). Like a power outage that gradually spreads from suburb to suburb, until the whole city is in a black out. The drop off starts in the visual areas of the brain (occipital lobe), then travels to the body sensation part of the brain (parietal lobe), then to the areas important in processing sound (temporal lobe).
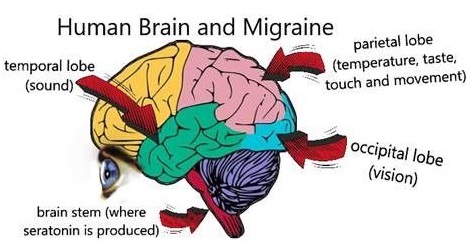
If there is a loss of activity in the visual areas of the brain, our eyes will still gather information important for sight, but our brain confuses the information and what we “see” will be distorted, disrupted and weird! When trying to get a grasp on ideas like this, it helps to remind ourselves that the eyes do not “see”. The eyes gather visual information about the outside world. This is then packaged into electrical and chemical messages that get sent along nerves to the occipital lobe in the brain. This information is then processed into something our brain can understand like a beautiful sunset or a busy city street.
If you want to learn more Dr Logan has written a blog – “How do we see: an inside look”.
Why are you more sensitive to light during a migraine or headache?
No one knows for sure, but if we look at the probable causes of migraine pain and photophobia, both processes stimulate the trigeminovascular system in the brain stem. It could be hypothesised that if this system is already stimulated by one of these two processes (say migraine pain), it will need less of the second stimulus (light) to achieve the same level of pain.
Photophobia is the word we use to describe when people have an increased sensitivity to light. This is when bright lights cause pain, that often feels like it is in or behind the eye. The exact translation of the word actually means fear of light.
Everyone is sensitive to light, but during a migraine your sensitivity to light can go off the chart. Migraines often force their sufferers into dark rooms. But once the migraine has passed, these afflicted individuals continue to be more sensitive to light than most.

Some interesting facts about photophobia;
- Other forms of headaches, including hangover headaches also show increased photophobia.
- It is common in depression and anxiety.
- Photophobia can occur in agoraphobia.
- Other eye conditions such as dry eye, viral keratoconjunctivitis, blepharospasm and more can also have increased light sensitivity.
- Photophobia can also occur in medical conditions unrelated to the eye, like chronic fatigue, fibromyalgia and head injuries.
- Short wavelengths of light (blue light) seem to create more discomfort than longer wavelengths. Blue light is found naturally in sunlight. As well as in screens, LED lights, CFL bulbs (energy saving bulbs) and fluorescent light bulbs.
- The darker your normal environment (e.g. you work in a darkened room) the more photophobic you are likely to be.
- People with light coloured eyes are more likely to have sensitivity to bright light than those with darker eyes.
Can sunglasses or tinted lenses help with photophobia and migraine?
Sunglasses are helpful for use in bright sunlight for most people. Sunglass wear indoors is also helpful for some patients while they are experiencing a headache, migraine or intense period of photophobia. However excess use of sunglasses, such as wearing them indoors under normal circumstances can be counterproductive. Excess wear can result in dark adaptation and dependency, this can result in pain being felt at lower levels of light than before.
FL-41 tinted spectacles have been successful in reducing migraine frequency in some studies. The tint is a pinkish-boysenberry colour. They have also been found to reduce feelings of photophobia between migraine attacks, but made no difference during migraine attacks. FL-41 tint filters out blue light, most likely found in fluorescent lights, reducing the flicker that people are often aware of.
Can poor eyesight trigger migraines?
Poor eyesight is not commonly a trigger for migraine. Although it can cause eyestrain (eye fatigue) and headaches in some people. Poor eyesight isn’t even in the top 10 most common causes of headaches!
Refractive errors, like astigmatism, myopia, hyperopia or presbyopia when uncorrected or under corrected can cause muscle tension. If you squint to see better, you are tensing the muscles in your forehead and around your eyes. Or you may find you lean closer to your computer screen, or lift your chin to try and see through the bottom of your spectacles. These changes to posture and muscle tension around the head, neck and shoulders is a very common cause of headaches. So, having up to date and properly fitting spectacles can actually reduce your muscle tension.
Despite this, when looking for the underlying cause of your headaches or migraines, having a full and thorough eye examination is still high on the list of priorities. Refractive errors may not be a common cause of headache or migraine, but they can contribute to the frequency and intensity of the head pain. There are also other eye related conditions that can cause visual disturbances or headaches such as Angle Closure Glaucoma and Age-Related Macular Degeneration.
What about in children?
Headaches in children are more likely to be caused by uncorrected visual issues compared to adults. So, a thorough eye examination for children with headaches, even with no complaints of poor vision is more likely to resolve the issue than in adults.

If you experience migraine headaches, we recommend consulting your doctor and/or eye care professional. They can help you get to the cause and come up with a treatment plan.
If you have any other questions or wish to book a consultation, get in touch with the team at Wellington Eye Centre. You can call us on 0800 733 327 or complete the contact form below.

What to expect during your Laser Suitability Medical Assessment at Wellington Eye Centre

Low-Level Light Therapy for Dry Eyes

Common Medications Used in Laser Eye Surgery

Amblyopia and Laser Eye Surgery